How Does The Dry, Thin Skin Of Elderly Individuals Affect The Absorption Rate Of Drugs?
Americans are aging at an unprecedented rate. Currently, the proportion of the population that is 65 years and older exceeds 12%, or almost 40 one thousand thousand.ane It is projected that this population volition grow significantly betwixt the years 2010 and 2050, especially the 65 and older group, which will more than double. This is largely due to the aging of the Baby Boomer generation who began turning 65 in January 2011. Age and chronic atmospheric condition are associated with increased utilize of healthcare.two Nurse practitioners in adult and family unit practise volition meet a larger proportion of older patients who nowadays a circuitous and potentially high-take chances group that will require medications.
 | Figure. No explanation bachelor. |
Prescribing safely and effectively for the older adult is contingent upon agreement the age-related changes that affect the pharmacodynamics and pharmacokinetics of drugs. Evidence-based guidance is express as there are few clinical trials that contain significant numbers of subjects over the historic period of 65. In fact, almost clinical drug trials that include older adults limit inclusion to the age range of 65 to 74; few include subjects over the age of 75.three-5 The prescriber must consider the effects of polypharmacy that put elderly patients at gamble for adverse drug events (ADEs), iatrogenesis, and drug interactions, too every bit the bug of adherence and cost. This commodity will discuss the effect of crumbling systems on the pharmacokinetics and dynamics of drugs, common problems that put the older patient at take a chance for ADE, strategies to ameliorate adherence, and models that guide the practitioner to safely and effectively prescribe for the elderly.
Normal changes in physiologic processes as well the equally the effects of acute and chronic conditions may significantly alter the fashion a drug is absorbed, distributed, metabolized, and eliminated in the crumbling patient. It is imperative that the prescriber consider these possible alterations in pharmacokinetics when treating a patient with medications to avoid iatrogenesis and ADE.6
Pharmacokinetics
Absorption. The effects of normal aging on the passive assimilation of drugs are not clear. Decreased acidity and function of mucosal cells in the stomach may affect the absorption of some drugs that require an acidic environment (such equally vitamin B12). Altered motility through the gastrointestinal (GI) tract and decreased blood catamenia to the bowel may all affect the absorption of oral medications, just the GI tract has such a large surface area that these effects are minimal.4,seven More often, information technology is concurrent therapy, such as antacids that create an alkaline metal environment, and anticholinergics that may contribute to decreased motion and interfere with the active transport of drugs into the torso.
Absorption of topical medications tin be afflicted past decreased hydration, tissue thickness, and surface lipids on the skin.7 Transdermal medications are designed for gradual absorption and rely on intact, well hydrated, healthy pare with adequate apportionment. Applying topical medications to nonintact skin tin profoundly increment the rate of absorption, while dry, thin skin without a good subcutaneous layer tin inhibit absorption of the drug. Suboptimal placement of transdermal medications can pb to an over- or undertreatment effect.
Distribution. In the older developed, drug distribution is affected by a number of age-related changes including a decrease in total body water and serum albumin while body fatty increases. Drugs that are water-soluble (such equally digoxin, theophylline) are distributed in a smaller surface area, and this may atomic number 82 to toxicity at the same dose that would be prescribed for a younger or center-anile adult. Similarly, drugs that are fat-soluble may accumulate in body fat, prolonging the outcome and resulting in ADE. This is especially hazardous with medications that affect the central nervous organization (CNS), such equally benzodiazepines.
Low serum albumin, a common finding in older adults, has the most significant effect on the distribution of medications. Many drugs are highly protein leap, and serum albumin is the principle plasma protein to which they bind. As less drug is bound to serum proteins, more than active drug is circulating freely in the serum competing for binding sites. Toxicity tin can quickly develop with drugs such as phenytoin, digoxin, and warfarin, putting the patient at risk for ADE. Upwards to 20% of hospital admissions for patients 65 years and older are related to the furnishings of medications.7,8
Metabolism. Nigh drugs are metabolized in the liver. With normal aging, the liver decreases in mass but besides in circulation.5,vii-10 Decreased blood flow is associated with decreased first pass metabolism, so more than drug is available in the bloodstream. This is the main reason that the elderly are prescribed a lower starting dose than the average adult. Information technology is important to exist enlightened of drugs expected to take a loftier rate of extraction upon first pass through the liver. Lidocaine, meperidine, morphine, propranolol, metoprolol, verapamil, nitrates, and barbiturates (such as phenobarbital) are amid the drugs with an elevated showtime pass effect.3,7,8 These medications, when prescribed at the usual starting dose, may cause significant ADE in an older developed with less vigorous hepatic circulation and resultant decreased first pass effect.
Elimination. Most drugs are eliminated through the renal system. The literature reveals a meaning variability of functional limitation in the kidney every bit a result of normal aging. Structural and biophysiologic changes include a decrease in the number of nephrons, bloodflow, and glomerular filtration charge per unit (GFR).3-5, 7-11 Creatinine clearance has often been used to measure out renal function. Creatinine is a byproduct of muscle tissue that is removed past the kidneys, making it an of import measure of renal function. Even so, with normal aging comes a marked subtract in lean muscle mass (sarcopenia), then older adults produce very lilliputian creatinine.five,7-10 Sarcopenia contributes to a reduced renal clearance of many drugs (such as digoxin, H2-receptor blockers, fluoroquinolones, penicillins, and aminoglycosides). It is best to consider the GFR, the accepted standard for measuring kidney function, when choosing both a drug and dose for renally impaired clients.
Pharmacodynamics
While pharmacokinetics considers how a drug is taken in, processed, and eliminated from the body, pharmacodynamics is the effect the drug has on the body itself.four,7,xi There are structural and physiologic changes in aging organ systems that can significantly influence the intended treatment effect. Reduced homeostatic responses, reduced tissue receptors, and changes in target organ sensitivity can influence drug result.
Central nervous system
A number of dynamic changes in the part and sensitivity of neuroreceptors occurs as a issue of normal aging, and this can have a significant clinical effect on medication therapy. There are a decreased number of neurons, a decreased cerebral blood menstruum, and an increase in the permeability of the blood-brain barrier, which exposes the patient to increased sensitivity to the therapeutic and toxic furnishings of drugs. Medications such as opioids, benzodiazepines, barbiturates, and drugs with anticholinergic action (such as diphenhydramine, clonidine) can result in cognitive harm, behavioral changes, and even delirium. Decreased activeness of dopamine-1 and dopamine-2 receptors tin produce extrapyramidal adverse reactions such as extreme restlessness and abnormal involuntary movements with the concomitant use of an antipsychotic and metoclopramide, an anitemetic.8,x
Cardiovascular system
Changes in the cardiovascular system tin can produce increased sensitivity, but few are reported to do so. However, decreased function of beta-adrenergic receptors can actually require increased amounts of certain drugs to reach desired therapeutic outcome, such as isoproterenol and beta-blockers.vii,thirteen,16 Baroreceptor role is impaired with aging and manifests clinically as a decreased ability to reach homeostasis through increased heart rate or vascular tone in the presence of low volume or position change. This has implications in the development of orthostatic hypotension, which puts the older patient at risk for falls and can exist exacerbated with antihypertensive medications or diuretics.
Other systemic changes
Impaired glucose regulation can put the older patient at chance for hypoglycemia when antidiabetic medications are prescribed. The prescriber should consider the possibility of an atypical presentation of hypoglycemia when presented with an older patient who exhibits somnolence or defoliation in the presence of an antidiabetic medication.7,8
Mutual problems that put elders at risk
Chronic atmospheric condition are mutual in an aging patient population, and there are often several comorbidities that require medication management. Polypharmacy, divers as the employ of ii or more medications, is frequent in the elderly population, particularly those residing in long-term-intendance (LTC) facilities. Older adults have a medication utilize rate that is 3 to iv times higher than younger adults.xviii About xx% of community-habitation elders are taking 10 or more medications; LTC facility residents represent an even larger percent of polypharmacy due to increased morbidity.eighteen This number of medications can be easily reached if exercise guidelines are followed for each chronic condition nowadays.15 Bear witness shows that clinical practice guidelines practice not provide for appropriate and quality care in the older adult with multiple comorbidities.6,eleven,15,16 These guidelines are designed for single conditions and do not consider the complexity of caring for a patient with several chronic diseases.
Patients are oft referred to specialty providers who prescribe concurrently with the primary care provider. Many patients exercise non communicate conspicuously with each provider; they may forget some of their medications or fail to mention over-the-counter, herbal, or dietary supplements they may be taking. Defoliation over the generic versus brand name of drugs can cause elderly patients to accept the same medication in two different forms, increasing the risk of ADE. The fact that older adults tend to have several chronic conditions and, in turn, are prescribed more medications automatically sets them up for potential interactions and ADE. Often, when an older patient is prescribed a medication, adverse reactions from the initial drug lead to the addition of other drugs to gainsay the undesirable effects leading to what is referred to as the "prescribing cascade."xiii,15,17,18
Functional limitations
The older patient may have difficulty with adherence to a medication regimen for a diversity of reasons. Cerebral harm can put a patient at adventure for either nether- or overtreatment. Patients may not attach if the medication schedule is too complicated, they exercise not sympathise the importance of completing the grade of a prescription, or if medications have similar sounding names.8,xiii Decreased visual acuity can make identification of medications hard and increase the likelihood of error in administration. Mobility can limit the older person's power to manage their medications in both procurement and assistants. The older patient may have barriers to transportation, being dependent on others for appointments and shopping, and may non be able to fill up a prescription in a timely manner. Arthritis or move disorders such as Parkinson'south disease can significantly impair the older adult's fine motor skills, limiting the ability to open the medication containers, handle small pills, or administer insulin.
Cost
Cost is often a significant cistron; up to 15% of older adults cannot afford their medications,7 don't fill prescriptions, or may accept fewer doses than what is prescribed. Medications that are no longer used may be kept to avoid waste and so used after their effectiveness has been significantly reduced. The elderly may share medications in an attempt to avoid a costly trip into the clinic. A common exercise to reduce price is pill splitting, either by the patient or pharmacy. Although this tin can significantly ease the burden of medication costs, non all medications are safe to dissever. Checking the manufacturer's prescribing information on the appropriateness of pill splitting is the safest practice.17
High-gamble medications
Older adults demonstrate important differences in the fashion their bodies handle medications and the furnishings those medications take on their bodies. The Beers Criteria,nineteen which was published equally original inquiry in 1991, updated in 1997,20 and revised in 2002,sixteen identified a number of drugs that were potentially inappropriate for the elderly. These drugs were determined to have a take chances for ADE that outweighed the potential therapeutic consequence.15,xvi,18 In fact, ii drugs which appeared on the original list are now off formulary including propoxyphene, which was plant to have little analgesic advantage over acetaminophen with far greater risk of ADE and meperidine, which has a high propensity for confusion.xvi This criterion has been used to evaluate care in LTC facilities, reduce the potential for ADE in older adults, and as a method for evaluating prescribing patterns for this population.fourteen,fifteen,16,18 While non all of these medications volition be discussed here, the more common and potentially dangerous drugs are addressed.
Anticoagulants are commonly prescribed and are drugs with the potential for the most serious consequences. Warfarin should be prescribed carefully, keeping the patient'southward dose at the lowest possible amount to achieve anticoagulation. Equally this drug is highly poly peptide bound, it is imperative that the prescriber monitor the serum total protein or albumin likewise as the prothrombin fourth dimension and international normalized ratio. Warfarin is metabolized in the liver, primarily through the CYP2C9 pathway.7 This pathway is used past a large number of other medications and concurrent utilize greatly increases the possibility of over-anticoagulation. Nearly notably are most antibiotics, antifungals, nonsteroidal anti-inflammatory drugs (NSAIDs), selective serotonin reuptake inhibitors, and many dietary or herbal supplements. If warfarin is necessary, use this medication at the everyman dose possible for the shortest duration that is feasible, and educate patients to tell any prescriber nearly their warfarin therapy prior to accepting any new or modify in current medications.
Medications with anticholinergic effects tin cause dry mouth, skin, and eyes, along with urinary memory and constipation. Of these agin reactions, urinary retention and constipation are amidst the about problematic for the older patient. Additionally, age-related changes in the CNS tin also predispose the older adult to excess sedation and falls, increased confusion, and delirium with psychosis. The older patient with cognitive impairment of any severity can be at loftier chance for psychosis with visual or auditory hallucinations. Information technology is important to annotation the presence of whatever existing medication with anticholinergic furnishings before prescribing another anticholinergic drug. These effects are cumulative, and if more than one drug is being used, it exponentially raises the risk. Some normally used medications with anticholinergic properties include antihistamines (chlorpheniramine, diphenhydramine), antidepressants (especially tricyclics such equally amitriptyline and nortriptyline), anti-parkinsonians (amantadine, benztropine), antidiarrheals, and antipsychotics.7,8,9 Antihistamines are not necessarily readily credible to the consumer when a combination drug is taken. For instance, a popular bedtime medication, Tylenol PM, contains diphenhydramine, which produces drowsiness.
Older patients are more sensitive to the effects of opioid pain medications. Sedation, anorexia, confusion, and constipation can become major problems when treating pain in the elderly. The American Elderliness Society recommends beginning with scheduled acetaminophen for balmy to moderate pain and so progressing to the lowest potency opioid if that method is ineffective.9,thirteen,18 NSAIDs are an option for unrelieved pain with acetaminophen, but the older adult is more likely to endure from GI inflammation and bleeding7,9 particularly if that patient has gastroesophageal reflux disease, peptic ulcer disease, or concurrent warfarin therapy (seeCommon weather condition and associated high-risk medications).
Improving adherence
Prescriptions that remain unfilled or taken incorrectly tin can also result in harm to the older patient. Initially, the best strategy to improve adherence is to have a complete list of current medications, including prescription, over-the-counter, dietary, and herbal supplements. Instruct the patient to bring in all of those items at the next appointment time, that is, "the brownish purse test."4,8,nine,10 It is during that appointment that an assessment of the patient's health literacy can be made. The patient should be able to tell the provider which medication is taken for what condition, the appropriate administration route and time, expected therapeutic effects, and adverse reactions that should exist reported.
When it is necessary to alter a medication regimen or prescribe a new drug, consider first if the new drug is absolutely necessary. Provide verbal and written instructions, non limited to the name of the drug and how often it should be taken, but also how it is expected to do good the patient, and when to report back to the prescriber if adverse reactions are experienced. Consider the toll, explore generic or less plush alternatives, and discuss the benefits and risks of adding a new drug with the patient and family. Chose a medication that is compatible with other medications currently taken, existing chronic conditions, and with the simplest assistants schedule. Once or twice daily medications will increase the likelihood that the patient will adhere to the regimen. Follow up with an appointment sooner than would exist expected with younger adults-the elderly tend to be more sensitive to medication effects and more probable to feel adverse reactions.iv,six,7,9,17
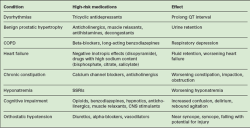 | Table Mutual weather condition and associated high-risk medications |
Models for safe and constructive prescribing
The precept in geriatric prescribing has long been "showtime depression, go slow." Another simple adage, "add ane-take one away," tin can also exist helpful. In improver, the American Medical Directors Association has developed guidelines for prescribing decisions for the older adult. This was based on the Beers Criteria20 just information technology is important to note that these criteria should exist used as a guide, inside a patient-centered, individualized approach. Prescription decisions should exist made based on testify forth with input from the patient and family, considering the health beliefs, prognosis, risk versus benefits, and quality of life.16
The prescriber might consider the acronym master when making prescribing decisions. This fix of rules for rational drug therapy is as follows:
* Minimize the number of drugs used
* Alternatives should always be considered, especially nondrug therapies
* Due southtart low and become slow
* Titrate therapy; adjust dose based on individual response
* Eastducate the patient and family unit; provide articulate, written instructions
* Review regularly; think that the older patient will demand closer monitoring.19
Another model for prescribing for the elderly is the CARE model.
"C" is for circumspection. Is the drug necessary or volition this condition resolve without medication? Use the lowest dose possible and prescribe for the shortest duration that is reasonable. "C" is also for compliance. Consider the grade (use liquid if the patient has difficulty swallowing), price, instructions, and functional limitations when ordering medication. "A" is for adjusting the dose for age. Older adults often need 1/4 to 1/two of the usual starting dosage. They also accept college levels of body fat versus lean muscle mass and lower albumin levels and so drugs that are fat soluble or highly protein bound need to exist adjusted downward. "R" is for review. Come across the older patient more ofttimes and review the drug regimen at every visit. Finally, "E" is for educate. Make sure the patient or family member understands what the medication is for, what the therapeutic effect should be, how long before it is expected to produce results, and what possible adverse reactions could occur.8 This is especially important so that the patient does not cease taking the medication assuming that it is non working.
Conclusion
Prescribing for the older adult is challenging, circuitous, and non without chance. Understanding the age-related changes that affect the pharmacokinetics and pharmacodynamics of drugs is the foundation of prescribing for the older adult. Chronicity, multiple comorbidities, functional limitations, polypharmacy, and toll tin can all put the older patient at risk for over- or undertreatment of their medical atmospheric condition. Farther, few clinical trials accept included the old-old (75+) when establishing risk and efficacy. Employing these strategies to improve adherence, reduce risk, and maximize outcomes will help the practitioner in safe and effective prescribing for the older patient.
REFERENCES
Source: https://www.nursingcenter.com/journalarticle?Article_ID=1262947&Journal_ID=54012&Issue_ID=1262784
Posted by: pippinfent1993.blogspot.com


0 Response to "How Does The Dry, Thin Skin Of Elderly Individuals Affect The Absorption Rate Of Drugs?"
Post a Comment